Day 1 :
Keynote Forum
Ham Benghuzzi
University of Mississippi Medical Center, USA
Keynote: The role of fibrous tissue thickness on the sustained release of biologicals from ceramic delivery systems
Time : 9:30

Biography:
Dr. Benghuzzi is a Professor at the University of MS Medical Center. He is known nationally and internationally as a pioneer in Ceramic Drug Delivery Systems. He has over 250 PubMed indexed articles and over 700 abstracts detailing the release characteristics of various biologicals from the bioceramic carriers. He has trained more than 35 PhD students who are actively involved in academic careers. He has mentored students at all levels (from high school, undergrad, grad, post doc and faculty). He has served as a mentor for residents and faculty on more than 10 funded grants. He has been in research leadership roles in many organizations such President of the Academy of Surgical Research, Vice President of the Rocky Mountain Bioengineering Society, President of MAS, Academy’s Executive Director, and also organized and chaired several regional, national and international society programs. He has also served on numerous NIH special emphasis panels including R-25, K01, KO8, T-35, and the P-60 center grants. In addition, he has received numerous awards from various organizations during his career. A few of his awards included: (1) The Presidential Award from the RMBS, (2) Presidential Award from SEM International, (3) the Endocrine’s Society Outstanding Investigator Award, (4) MAS Contribution to Science Award, (5) The MAS Dudley Peeler Award, and (6) HEADWAE Award, (7) C. Hall Award, Outstanding Contribution to Biomedical Engineering (32nd SBEC), and (8) ISCM Excellence Award from the International Society for Ceramics in Medicine. He was invited as a keynote/plenary to speak at state, national and international levels including recent invitations in France, Italy, Spain, Greece, China, Poland, Dubai and Canada. He is a fellow of the American Institute for Medical and Biological Engineering (AIMBE) as well as an International Fellow of Biomaterials Science and Engineering (FBSE).
Abstract:
Keynote Forum
Guoxiong Xu
Fudan University, China
Keynote: Role of pyridoxine 5'-phosphate oxidase in breast cancer
Time : 10:55-11:35

Biography:
Guoxiong Xu is a Professor of Oncology, Scientist, and Director of Research Center for Clinical Medicine in Jinshan Hospital, Fudan University, China. He obtained MD from the Faculty of Medicine, Shanghai Second Medical University in China, a master’s degree in Medical and Pharmaceutical Research from the Free University of Brussels in Belgium, and a Ph.D. degree from York University in Canada. He has worked as a Clinician and Research Scientist in several reputed universities and institutes. He has published more than 80 papers in peer-reviewed journals and his work has been supported by grants such as the National Natural Science Foundation of China. He has been serving as a member of the Editorial Board in many scientific journals.
Abstract:
Breast cancer is the most common malignant tumor and the second leading cause of cancer death in women worldwide. Among all breast cancer cases, invasive ductal carcinoma (IDC) is the most common type of breast cancer that accounts for more than 70% of total diagnosed cases. Pyridoxine 5'-phosphate oxidase (PNPO) is a converting enzyme for pyridoxal 5'-phosphate (PLP), an active form of vitamin B6, which serves as a co-factor for more than 140 enzymes that participate many metabolic reactions. However, the biological function of PNPO in human breast IDC remains unclear. Furthermore, a regulatory mechanism of PNPO is not fully understood. Recently, we evaluate the biological function and regulatory mechanism of PNPO in human IDC. We found that PNPO was associated with IDC development and was correlated with the overall survival of patients. Loss-of-function assays showed that PNPO affected breast cancer cell proliferation, migration, invasion, colony formation, cell cycle, and apoptosis. Interestingly, we found a microRNA response element in PNPO and lncRNA MALAT1 transcripts for miR-216b-5p. Dual-luciferase reporter assays confirmed the binding of miR-216b-5p to PNPO and MALAT1. Targeting MALAT1 resulted in the alteration of the expression level of miR-216b-5p and PNPO mRNA. The change of miR-216b-5p level affected PNPO expression, indicating that PNPO was regulated by MALAT1 via miR-216b-5p. These results reveal a regulatory mechanism of competing endogenous RNAs in breast cancer.
Keynote Forum
Michelle A. Tucci
University of Mississippi Medical Center, USA
Keynote: Development of a rat neuroma model to study hyperalgesia and the histopathological changes associated with pain
Time : 11:35-12:15

Biography:
Painful neuromas are a common and debilitating result of peripheral nerve trauma and a common complication following limb amputation. We sought to evaluate early developing and mature neuromas tissue for specific subtypes of fibers and receptors based on their immuno-reactive profiles. Our overall goal was to identify the location of the NPY producing cells and the density of NPY 1 receptor on the growing neuroma tissue. Neuropeptide Y is a 36 amino acid peptide that has been implicated in pain and the NPY 1 receptor is believed to contribute to the growth of the neuroma. The results show by 30 days the presence of a neuroma that increased in size over 60 days. Within seven days of injury the pain withdrawal threshold declined by 73% while an average decline in the Sham injured animal group declined 33%. The decline in the Sham group was most likely due to inflammatory pain from the surgical site. By 30 days the animals in the Sham group showed no differences in pain threshold measurements either between legs or compared to the control Naïve animals. The CCI animals showed a slight rebound in pain threshold withdrawal to 43% of their baseline score. Similar finding were seen at the 60 day time point. Detection of the NPY 1 receptor was seen surrounding the epineurium and the cells positive for NPY were within the fat surrounding the nerve and with the cells of perineum. Overall, our findings show NPY producing cells in the expanding region of the neuroma. Future research will be directed at targeting the receptors to disrupt growth and/or development of the neuroma.
Abstract:
Painful neuromas are a common and debilitating result of peripheral nerve trauma and a common complication following limb amputation. We sought to evaluate early developing and mature neuromas tissue for specific subtypes of fibers and receptors based on their immuno-reactive profiles. Our overall goal was to identify the location of the NPY producing cells and the density of NPY 1 receptor on the growing neuroma tissue. Neuropeptide Y is a 36 amino acid peptide that has been implicated in pain and the NPY 1 receptor is believed to contribute to the growth of the neuroma. The results show by 30 days the presence of a neuroma that increased in size over 60 days. Within seven days of injury the pain withdrawal threshold declined by 73% while an average decline in the Sham injured animal group declined 33%. The decline in the Sham group was most likely due to inflammatory pain from the surgical site. By 30 days the animals in the Sham group showed no differences in pain threshold measurements either between legs or compared to the control Naïve animals. The CCI animals showed a slight rebound in pain threshold withdrawal to 43% of their baseline score. Similar finding were seen at the 60 day time point. Detection of the NPY 1 receptor was seen surrounding the epineurium and the cells positive for NPY were within the fat surrounding the nerve and with the cells of perineum. Overall, our findings show NPY producing cells in the expanding region of the neuroma. Future research will be directed at targeting the receptors to disrupt growth and/or development of the neuroma.
Keynote Forum
Amr Rajab
LifeLabs, Canada
Keynote: Ten-color 15-antibody flow cytometry panel for immunophenotyping of lymphocyte population
Time : 12:15-12:55

Biography:
Amr Rajab is a registered member of the Canadian Society for Medical Laboratory Science (CSMLS), the College of Medical Laboratory Technologists of Ontario (CMLTO), and he holds Qualification in Cytometry (QCYM) from the American Society for Clinical Pathology, Board of Registry (ASCP). He conducted several overseas training sessions at Hospitals affiliated and also conducted courses in conjunction with the ICCS/ESCCA Bi-Society in 2015. He is a member of the ICCS Education Committee and also a member of the Hematology Scientific Committee of the Canadian Institute for Quality Management in Health (IQMH). He developed a special interest in hemato/lymphoid malignancies and enjoyed establishing the diagnosis on the submitted blood and bone marrow smears based on morphological assessment and special stains
.
Abstract:
We have developed a lymphoproliferative disorder screening tube (LPD-ST) with the aim to provide comprehensive immunophenotyping of lymphocyte subsets with minimal need for additional testing. The LPD-ST consists of CD4/kappa FITC, CD8/lambda PE, CD3/CD14ECD, CD38PC5.5, CD20/CD56PC7, CD10APC, CD19APC-A700, CD5APC-A750, CD57/CD23PB and CD45KO. The LPD-ST was validated against previously used lymphocyte subset panels in Canada (n=60) and in Sweden (n=43) and against the OneFlow™ LST (n=60). The LPD-ST panel was then implemented in clinical practice using dried monoclonal antibody reagents (Duraclone®) on 649 patient samples in Sweden. In 204 of 649 samples (31%), a monotypic B-cell population was found. Of these cases, a final diagnosis could be rendered in 106 cases (52%), and in the remainder, additional B-cell immunophenotyping was performed. In 20 (3%) samples, an aberrant T-cell population was confirmed by additional testing. Of 425 samples diagnosed as normal/reactive lymphoid tissue, 50 (12%) required additional immunophenotyping, mostly due to an abnormal CD4/CD8 ratio. The LPD-ST tube significantly minimizes the need for additional testing, improves the turn-around time, and reduces the cost of LPD immunophenotyping. It is also suitable for investigating paucicellular samples such as cerebrospinal fluid or fine needle aspirates.
Keynote Forum
Amr Rajab
LifeLabs, Canada
Keynote: Ten-color 15-antibody flow cytometry panel for immunophenotyping of lymphocyte population
Time : 10:55-11:35

Biography:
Amr Rajab is a registered member of the Canadian Society for Medical Laboratory Science (CSMLS), the College of Medical Laboratory Technologists of Ontario (CMLTO), and he holds Qualification in Cytometry (QCYM) from the American Society for Clinical Pathology, Board of Registry (ASCP). He conducted several overseas training sessions at Hospitals affiliated and also conducted courses in conjunction with the ICCS/ESCCA Bi-Society in 2015. He is a member of the ICCS Education Committee and also a member of the Hematology Scientific Committee of the Canadian Institute for Quality Management in Health (IQMH). He developed a special interest in hemato/lymphoid malignancies and enjoyed establishing the diagnosis on the submitted blood and bone marrow smears based on morphological assessment and special stains
.
Abstract:
We have developed a lymphoproliferative disorder screening tube (LPD-ST) with the aim to provide comprehensive immunophenotyping of lymphocyte subsets with minimal need for additional testing. The LPD-ST consists of CD4/kappa FITC, CD8/lambda PE, CD3/CD14ECD, CD38PC5.5, CD20/CD56PC7, CD10APC, CD19APC-A700, CD5APC-A750, CD57/CD23PB and CD45KO. The LPD-ST was validated against previously used lymphocyte subset panels in Canada (n=60) and in Sweden (n=43) and against the OneFlow™ LST (n=60). The LPD-ST panel was then implemented in clinical practice using dried monoclonal antibody reagents (Duraclone®) on 649 patient samples in Sweden. In 204 of 649 samples (31%), a monotypic B-cell population was found. Of these cases, a final diagnosis could be rendered in 106 cases (52%), and in the remainder, additional B-cell immunophenotyping was performed. In 20 (3%) samples, an aberrant T-cell population was confirmed by additional testing. Of 425 samples diagnosed as normal/reactive lymphoid tissue, 50 (12%) required additional immunophenotyping, mostly due to an abnormal CD4/CD8 ratio. The LPD-ST tube significantly minimizes the need for additional testing, improves the turn-around time, and reduces the cost of LPD immunophenotyping. It is also suitable for investigating paucicellular samples such as cerebrospinal fluid or fine needle aspirates.
- Diagnostic Cytopathology | Cancer Cytopathology | Histopathology
Session Introduction
Manjit Singh Bal
Maharishi Markandeshwar Medical College & Hospital, India
Title: Histopathological findings in nephrectomy specimens: A study of 50 cases

Biography:
Dr. Manjit S. Bal is MBBS & MD (Pathology) from GMC Amritsar (India), has a fellowship (FICP) in Pathology. He retired after >37 years of govt. job, >31 years as faculty and 17 years as Head Pathology at Patiala. Currently, he is professor Pathology in a Pvt. Medical College. Areas of interest-Histopathology, Cytology, Oncopathology, had trained 115 postgraduates and published 116 papers in reputed journals, has been serving as an editorial board member. He is a regular columnist of health articles in Punjabi for Indian & over sea news-papers/magazines, has authored 12 books in Punjabi, English & Hindi on health topics and literary, has also produced two films on his own stories, script, music and lyrics. He has travelled widely in India USA, Canada, Australia, Singapore, Middle East)
Abstract:
Though ultrasound and CT have improved the diagnosis of renal lesions, explorations for a presumptive diagnosis of renal cell carcinoma (RCC) has to be done and are found to have other pathology. Histopathological examination of nephrectomies is of utmost importance for confirming the pre-operative diagnosis, typing of cancer.
Nephrectomy is the surgical removal of a diseased or damaged kidney. Simple nephrectomy is done for transplant purpose. Radical nephrectomy involves removal of a kidney, a part of the ureter, adrenal gland and fatty tissues surrounding the kidney. Nephrectomy is indicated
- Non-functioning or very poorly functioning hydronephrotic, infected, ischemic, stone-containing-kidney with a normal kidney on the other side.
- Malignant neoplasm of kidney i.e. Renal Cell Carcinoma, Nephroblastoma, Transitional Cell Carcinoma.
- Renal Tuberculosis/actinomycosis with resistant organisms involving the whole of the Adult Polycystic Kidney disease.
- Severely Traumatic Kidney.
- Congenital abnormalities of Kidney.
- Harvesting of the kidney from a Kidney Donor.
This paper is based on the histopathological analysis of lesions of a kidney in fifty nephrectomies received in the Department of Pathology at Government Medical College Patiala (India). Of the total cases, 40% were neoplastic and 60% were non-neoplastic. Neoplasms include two benign lesions (Renal Hemangioma & Renal Papillary adenoma, one case each); eighteen cases of malignant tumours i.e. RCC-11, Nephroblastoma-3, TCC-3 & Metastatic-1.
Non-Neoplastic lesions (30) were Chronic Pyelonephritis-26, Xanthogranulomatous CPN-1, Tuberculosis-1, Renal Amoebic abcess-1 and Traumatic Kidney-1.
Gross and microscopic findings were critically observed and recorded. We observed that nephrectomy could be avoided in benign lesions.
Kevin Kuan
Albert Einstein College of Medicine, USA
Title: Hepatoid adenocarcinoma of the lung: A cause of diagnostic pitfall
Biography:
Kevin Kuan after receiving his degree in Bachelor of Science in Pharmacology and Mathematics, he got enrolled in St. George’s University, West Indies, for his further education in medicine. As part of the program curriculum, he was exposed to different kind of medical systems and practices, including the local Grenadine Hospital, National Health Service in the United Kingdom, and various hospitals in Chicago. Currently, he is working as a Resident Physician at Montefiore Medical Center/Albert Einstein College of Medicine, Department of Pathology.
Abstract:
Background: Hepatoid adenocarcinoma of the lung (HAL) is a recently recognized adenocarcinoma variant. It is exceedingly rare and often takes on an aggressive clinical course. Although the histologic features of HAL have been well documented in the literature, there are only rare case reports describing the cytomorphologic features of this entity. Here, we present a case of HAL associated with metastatic pleural effusion.
Case Presentation: A 47-year-old man with a history of heavy smoking, presented to the emergency department complaining of localized chest pain for 3 weeks duration. Imaging studies revealed a large apical fluid-filled bulla in the right lobe, with underlying dense nodularity. A clinical picture of malignancy with superposed infection was favored, and CT- guided core needle biopsy ensued. The biopsy showed malignant cells arranged in trabeculae and cords, with abundant eosinophilic cytoplasm and centrally placed nuclei. Immunohistochemical stains were positive for CK7, EMA, pCEA, HEPAR-1 and negative for TTF-1, CK20, NapsinA, and AFP. The diagnosis of HAL was made, and the patient underwent right upper lobectomy. Despite surgical intervention, the patient developed the metastatic disease of the pleural. The fine needle aspiration was performed and revealed poorly cohesive hepatoid malignant cells, with prominent nucleoli, abundant eosinophilic cytoplasm and focal intra-cytoplasmic bile, consistent with the metastasis from the lung primary.
Conclusion: Hepatoid adenocarcinoma of the lung is a rare and aggressive tumor that requires an accurate and timely diagnosis. This case demonstrates the cytomorphologic features and immunohistochemical stains that can be performed on cytopathology specimens to diagnose this tumor and avoid the pitfall of diagnosing it as a Hepatocellular carcinoma.
Biography:
Abstract:
In cases of severe hypercalcemia with greater than 14mg/dl the possibility of malignancy has to be considered. Multiple myeloma cells will increase the release of macrophage inflammatory protein 1 alpha and tumor necrosis factor, which are inflammatory proteins that cause an increase in macrophages which cause an increase in calcitriol. The organs that are frequently affected by the proliferation of plasma cells include kidneys and bone. Kidneys are affected because of the increase in the abnormal protein being filtered through the kidneys that leads to the formation of cast and damage to the glomerulus filtration barrier, which will lead to acute kidney damage 2.
Case Report: A 54-year-old morbidly obese African American female with a medical history of hypertension, anemia, and uterine fibroids presented to the emergency department with generalized abdominal pain for 3 days. The patient rated the pain at five out of ten and described it as a dull cramping pain that waxed and waned. The pain was non-positional and had not been alleviated by anything. She stated that she had nausea associated with the pain and one episode of vomiting. She also had some constipation before the onset of pain. The pain did not radiate anywhere. She denied any recent trauma, diarrhea, fevers, weakness, shortness of breath, chest pain, or any other muscle pains. She also denied having this pain in the past or any recent travel or changes to her current diet. She had some unintentional weight loss but she was not certain how much. She had no prior surgical history. She denied any tobacco, alcohol, or illicit drug use. Vital signs on admission, the patient’s temperature was 97.8°F, heart rate was 100 beats/min, blood pressure was 136/64, respiratory rate was 18 breaths/min, and oxygen saturation was 97%. On physical exam, the patient was alert and oriented Å~3, with mild discomfort but no distress. Her lungs were clear to auscultation with no wheezing or crackles appreciated. Her heart rate and rhythm were regular with no extra heart sounds or murmurs. Her abdomen had normal bowel sounds in all four quadrants, with tenderness upon palpation around the epigastric area, but with no signs of guarding or rebound tenderness. The laboratory test results from the emergency room. Values to note are the patient’s hemoglobin/hematocrit of 8.2/26 and the mean corpuscular volume of 107. The BUN/creatine of 33/3.6 was a significant increase from her last laboratory test result of 16/0.75 from 6 months earlier. The patient’s calcium level was 18.4mg/dL (range, 8.4–10.2mg/dL) with albumin was 3.3g/dL (range, 3.5–5g/dL). Her corrected calcium level was 19mg/dL. The patient’s laboratory results were consistent with macrocytic anemia, hypercalcemia, and acute kidney injury. The patient’s chest X-ray showed no acute cardiopulmonary process. The abdominal CT showed neither masses nor renal stones. The EKG showed sinus tachycardia. The patient’s serum PTH level was decreased to 11pg/mL (normal, 15–65pg/mL), while her PTHrP levels were slightly elevated at 3.4pmol/L (normal, <2.0). Protein electrophoresis was also performed, showing an M spike of 0.2 (0). The patient’s activated vitamin D level was <5ng/mL (normal, 19.9–79.3ng/mL), vitamin A was 7.2mg/dL (normal, 33.1–100mg/dL), TSH was 1.21mIU/L (normal, 0.47–4.68mIU/L), and free T4 was 1.27ng/dL (normal, 0.78–2.19ng/dL). Urine samples were sent out to test for Bence Jones protein, kappa light chains, and lambda light chains. Immune electrophoresis was done as well with the suspicion of multiple myeloma higher in the differentials after the recent information obtained. The patient was found to have Bence Jones protein present in the urine with her electrophoresis coming back positive for an increase in kappa light chains of 806.7mg/L (n=0.33-1.94), with a normal lambda light chain of 0.62mg/L (n=0.57-2.63). Her IgG levels were also low 496mg/dL (n=610-1660). Patients’ bone marrow biopsy performed revealing plasma cells greater than 10 percent.
Discussion: In severe hypercalcemia with a value of greater than 14 the possibility of malignancy has to be addressed. Patients who develop hypercalcemia from malignancy tend to have a worse prognosis. The treatment has to be initiated in an appropriate time manner because delays can lead to severe complications such as arrhythmias, acute kidney injury, and seizures. The first step in management is IV hydration to have a urine output of 150mL/hr and then consider combined calcitonin and bisphosphonate treatment in patients. In refractory cases, in which the calcium will not respond to treatment consider using glucocorticoids and denosumab. Multiple myelomas will affect the bones by causing osteolytic lesions. This occurs by increased activation of osteoclast via RANKL and the down-regulation of osteoblast by decreasing OPG7. The patient illustrated lytic lesions in 2 of her left lower ribs, in both of her forearms and femurs. Kidneys are typically affected because of the increase in the abnormal protein being filtered through the kidneys that eventually lead to the formation of cast and damage to the glomerulus filtration barrier, which will cause an increase in creatine ratio and lead to acute kidney damage 2. This phenomenon was observed in this patient and the damage became so severe that hemodialysis was required. This posed a great challenge because of the need to give fluids to help reduce her calcium while managing her acute kidney injury status, created the need for constant monitoring. Which posed a great risk for the patient in the delay of reducing her calcium levels without causing permanent damage to her kidneys.
Katherine Cochrane
University of Tennesee, USA
Title: Transformation of myelodysplastic syndrome to acute lymphoblastic leukemia: A case report

Biography:
Dr. Katherine Cochrane is a PGY-3 in the Department of Pathology at University of Tennessee Medical Center in Knoxville, TN. She is a native of Calgary, Alberta and is a graduate of Medical University of the Americas.
Abstract:
Myelodysplastic syndrome (MDS) comprises a heterogeneous group of clonal hematopoietic cell disorders characterized by cytopenias, morphologic abnormalities, ineffective hematopoiesis, and increased risk of transformation to acute leukemia. Acute leukemia evolving from MDS is usually of myeloid lineage, while transformation into acute lymphoblastic leukemia (ALL) is extremely rare. We present the case of a 73-year-old Caucasian male who was found to have pancytopenia on routine blood work. He continued to have progressive pancytopenia requiring intermittent transfusions. Subsequent bone marrow biopsy revealed hypocellular bone marrow with dyserythropoiesis and increased blasts. A diagnosis of MDS with excess blasts (MDS-EB2) was rendered. Three cycles of hypomethylating therapy were administered before treatment was discontinued due to severe cytopenias. Repeat bone marrow biopsy showed normocellular marrow comprised of 50% moderate to large sized blasts with high nuclear to cytoplasmic ratios and prominent nucleoli. Aberrant immunophenotype with expression of CD19 and TdT was consistent with B-cell ALL. Retrospective review of the initial bone marrow biopsy revealed occasional blasts with lymphoid morphology, as well as variable expression of CD19. These findings suggest a biphenotypic cell population at the time of initial MDS diagnosis with expansion of the clonal lymphoid population, while undergoing hypomethylating agent therapy. Due to the patient’s poor performance status, he was unable to receive further treatment and died within a month of the second biopsy. The bilineage cell population supports the theory that MDS arises from a pluripotent precursor cell with chemotherapy regimen possibly responsible for alteration of the clonal evolution.
Jacob Amsalu Bayisa
National Taiwan University of Science and Technology, Taiwan
Title: Automatic cervical pre-cancerous cell detection from pap smear samples using deep learning

Biography:
Jacob Amsalu Bayisa is a current graduate student at the National Taiwan University of Science and Technology in Taiwan. He is studying his Masters in Biomedical Engineering and his research area is Biomedical Imaging. In Ethiopia, he was serving as an Emergency Surgery and Obstetrics Officer and he has solid 5 years of clinical experience.
Abstract:
According to the 2018 WHO cancer report, cervical cancer is the fourth commonest type of cancer in women. For early screening of cervical cancer pap test and liquid cytology are commonly used, and diagnosis of pre-cancerous cells heavily relies heavily on the experience of the clinician for an accurate diagnosis. The collected cells are manually scanned under the microscope by a pathologist. Especially in developing countries, there is a shortage of clinicians and screening service is largely unavailable. Nowadays a subtype of machine learning called deep learning technologies is heavily being implemented for various clinical purposes. We developed an automatic cervical pre-cancerous cell detection technique using a deep learning model, that can be used for screening of cervical cancer. For training of our model, we used pap smear picture data which was collected from the DTU/Herlev Pap Smear Databases which contains 917 pap smear images. We used 80% of data for training and 10% for validation and 10% for tests. We also used the data augmentation method using the generative adversarial network to enhance model generalization. Our deep learning model is similar to U-Net structure and was able to detect precancerous cell with an accuracy of 94% which is a state of the art performance and can be used for automatic screening of cervical cancer. The trained model can also be easily deployed to a portable device like mobile phones and tablets.
Aleksandra Zuraw
Charles River Laboratories Montreal, Canada
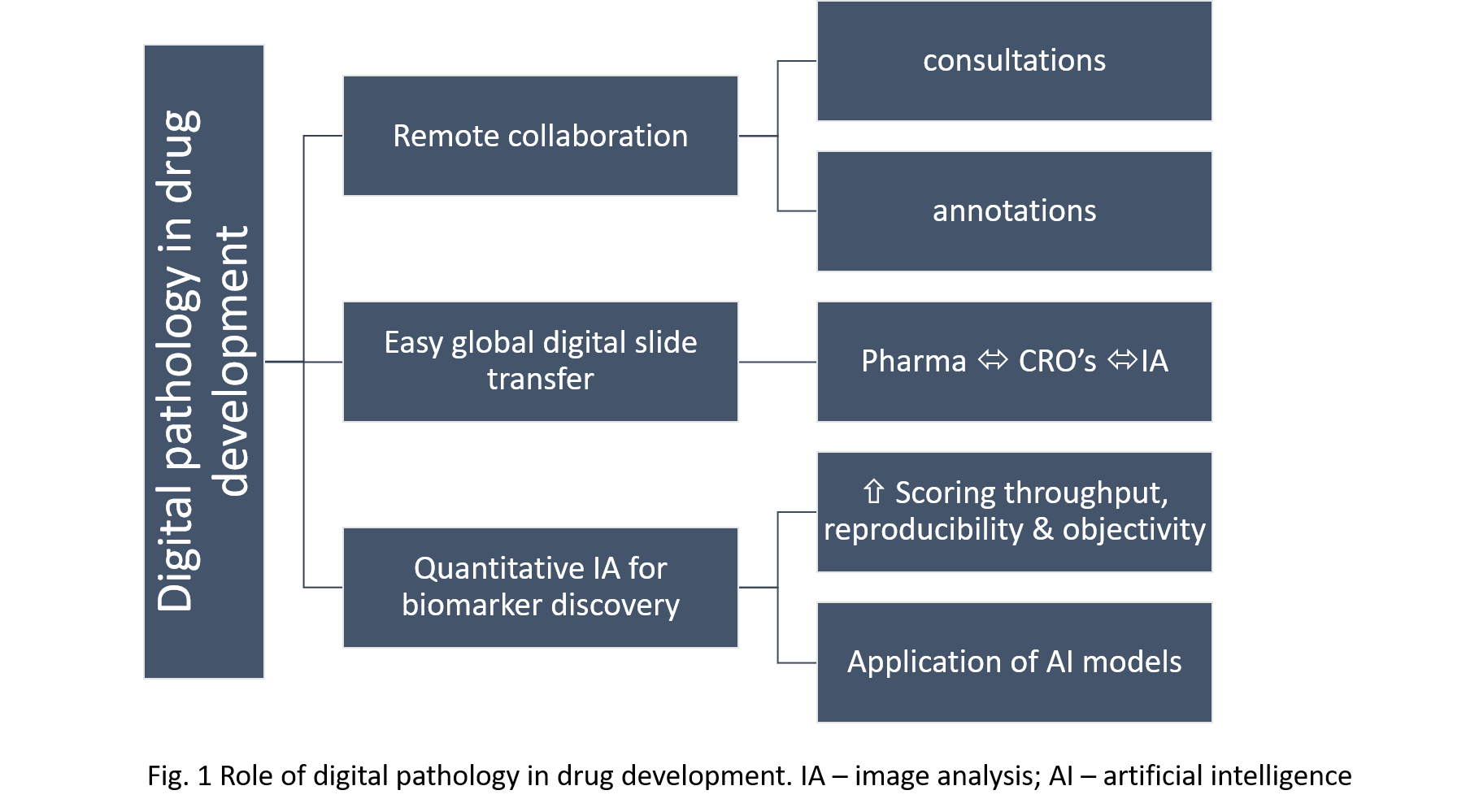
Title: Role of digital pathology in drug development process

Biography:
Aleksandra Zuraw is an ACVP board-certified veterinary pathologist with extensive experience in applying digital pathology to drug development. She is currently a Veterinary Pathologist at Charles River Laboratories Montreal, Canada. In addition to histopathological evaluation of pre-clinical animal studies, she has extensive expertise in digital image analysis powered quantification of immune-oncology tissue biomarkers and has worked closely with computer scientists and translational scientists to provide support for the drug development process. She obtained her DVM from the Wroclaw University of Environmental and Life Sciences, Poland and her PhD at the Freie Universität in Berlin, Germany.
Abstract:
Digital pathology is the process of performing pathology services using computers and digital images instead of microscopes and glass slides. With the increasing capabilities of pharmaceutical companies and contract research organizations to rapidly perform whole slide imaging and convert glass slides into digital images, there is a great potential to unlock the benefits of this technology for the drug development process. Pathologists are crucial members of drug development teams and are engaged in every step of the process, contributing significantly to the discovery, preclinical and clinical phases. Implementation of digital pathology workflows within and across organizations empowers them and benefits the drug development process in multiple ways. Often pathologists involved in pharmacological studies are geographically dispersed. The use of digital pathology allows them to communicate fast and perform slide consultation in real time regardless of location, which increases the efficiency of their work. Multiple pathologists can view, annotate and comment on the same slide simultaneously. The digitization of slides enables image analysis-powered quantitative measurements of biomarkers, lesions and abnormalities, which increases the throughput, reproducibility and objectivity of pathologists’ scoring. As tissue research is cross-disciplinary, access to digital pathology for different groups involved in drug development, especially the DVM and MD pathologists, helps them work more collaboratively and better understand their contributions. This technology is still considered novel, and in many institutions, its implementation is met with skepticism. Nevertheless, making it accessible and user-friendly for pathologists, standardizing it and applying it broadly across organizations, will undoubtedly accelerate and advance drug development.

Biography:
Dr. Alice Zemljic-Harpf has obtained her Medical Degree from the Medical University Graz, Austria in 1997. She conducted her postdoctoral studies in molecular cardiology at the Cedars-Sinai Medical Center Los Angeles (1999-2000), UCLA (2000-2003) and UCSD, School of Medicine. She is the director of The Cardiovascular Physiology and Imaging Unit at the Cardiac/Neuro Protection Laboratories at UCSD, Department of Anesthesiology. She has published 24 papers in high-impact pier reviewed journals (Circulation, Circulation Research, Glia, Cerbarl Cortex, The FASEB Journa, Heart Rhythm, The American Journal of Pathology, etc.). Her most recent work on atoravstatin induced adverse events gains international attention.
Abstract:
Background: Statins are amongst the most widely prescribed drugs to reduce LDL-cholesterol for the treatment of cardiovascular disease. Approximately one in five people in the United States between the ages of 45 and 75 take a statin. Like all drugs, statins can cause harmful side effects, such as muscle pain/weakness (statin myopathy), fatigue, nerve pain, and cognitive impairment. Because statin-induced myopathy is known to be associated with reduced oxidative phosphorylation in mitochondria of skeletal muscle we hypothesized that similar effects would occur in cardiac muscle.
Methods and Results: When male mice underwent atorvastatin and pravastatin administration per os for up to 7 months, only long-term atorvastatin, but not pravastatin administration induced: 1) elevated serum creatine kinase, 2) swollen, misaligned, size variable, and disconnected cardiac mitochondria, 3) altered ER-structure, 4) repression of mitochondrial and endoplasmatic reticulum related genes, and 5) 21% increased mortality in cardiac-specific vinculin knockout- mice.
Neonatal cardiac ventricular myocytes were treated with atorvastatin and pravastatin for 48hours. Both statins induced ER-stress, but only atorvastatin: 1) inhibited of ERK1/2T202/Y204, AktSer473 and mTOR signaling, 2) reduced protein abundance of caveolin-1, dystrophin, epidermal growth factor receptor and insulin receptor-β, 3) decreased RhoA activation, and 4) induced apoptosis. In cardiomyocyte-equivalent HL-1 cells atorvastatin, but not pravastatin, reduced mitochondrial oxygen consumption.
Conclusion and Clinical Implication: Skeletal muscle biopsies from patients with statin myopathy show increased lipid storage and alters mitochondrial structure. We are the first to demonstrate in vivo that long-term atorvastatin administration altered cardiac ultrastructure, a finding with important clinical implications.
Amr Rajab
LifeLabs, Canada
Title: Ten-color 15-antibody flow cytometry panel for immunophenotyping of lymphocyte population

Biography:
Amr Rajab is registered member of the Canadian Society for Medical Laboratory Science (CSMLS), the College of Medical Laboratory Technologists of Ontario (CMLTO), and I hold Qualification in Cytometry (QCYM) from the American Society for Clinical Pathology, Board of Registry (ASCP). He conducted several overseas training sessions at Hospitals affiliated and also conducted courses in conjunction with the ICCS/ESCCA Bi-Society in 2015. He is a member of the ICCS Education Committee and also a member of the Hematology Scientific Committee of the Canadian Institute for Quality Management in Health (IQMH). He developed special interest in hemato/lymphoid malignancies and enjoyed establishing the diagnosis on the submitted blood and bone marrow smears based on morphological assessment and special stains.
Abstract:
We have developed a lymphoproliferative disorder screening tube (LPD-ST) with the aim to provide comprehensive immunophenotyping of lymphocyte subsets with minimal need for additional testing. The LPD-ST consists of CD4/kappa FITC, CD8/lambda PE, CD3/CD14ECD, CD38PC5.5, CD20/CD56PC7, CD10APC, CD19APC-A700, CD5APC-A750, CD57/CD23PB and CD45KO. The LPD-ST was validated against previously used lymphocyte subset panels in Canada (n=60) and in Sweden (n=43) and against the OneFlow™ LST (n=60). The LPD-ST panel was then implemented in clinical practice using dried monoclonal antibody reagents (Duraclone®) on 649 patient samples in Sweden. In 204 of 649 samples (31%), a monotypic B-cell population was found. Of these cases, a final diagnosis could be rendered in 106 cases (52%), and in the remainder, additional B-cell immunophenotyping was performed. In 20 (3%) samples, an aberrant T-cell population was confirmed by additional testing. Of 425 samples diagnosed as normal/reactive lymphoid tissue, 50 (12%) required additional immunophenotyping, mostly due to an abnormal CD4/CD8 ratio. The LPD-ST tube significantly minimizes the need for additional testing, improves the turn-around time, and reduces the cost of LPD immunophenotyping. It is also suitable for investigating paucicellular samples such as cerebrospinal fluid or fine needle aspirates.
Jamshid Abdul-Ghafar
French Medical Institute for Mothers and Children (FMIC), Afghanistan
Title: Hepatoid adenocarcinoma of the lung: A cause of diagnostic pitfall

Biography:
Dr. Jamshid Abdul-Ghafar has his expertise in Histopathology and Cancer research. He has done his M.D. degree in Afghanistan. He has joined Yonsei University, Wonju College of Medicine in South Korea for his Ph.D. in the Department of Pathology. He is currently working at French Medical Institute for Mothers and Children (FMIC) in Kabul, Afghanistan. Besides being a Pathologist, he has involved in Research and Academic works as well. He is working as Administrator of Postgraduate Medical Education and Program Director for Pathology residents. He has published more than 15 articles in different international science-indexed journals.
Abstract:
Introduction: Malignant mesothelioma (MM) is well known as aggressive cancer which has the resistance to usual treatments and show poor prognosis. Little has been reported regarding the effective therapeutic methods of MM. Recently, epidermal growth factor receptor (EGFR) gene has been introduced that it has important role in the biologic features and tumor growth of the pleural MM, and the novel therapeutic agent such as EGFR tyrosine kinase inhibitor attempt to treatment of MM. We evaluated the expression of EGFR gene using Immunohistochemical stains (IHC), fluorescence in situ hybridization (FISH), and EGFR gene mutation in cases of MM of Korean patients. Methods: We reviewed clinicopathologic findings for 44 cases. The mean age of cases (male 32, female 12) was 59 years old (19-79). Most cases were occurred in the pleura (38 cases, 83.4%) and 6 cases (13.6%) from the peritoneum. The IHC for EGFR antibody for 29 cases, FISH analyses for 17 cases and detection of EGFR gene mutation for 36 cases were performed. The histologic subtypes were epithelioid in 31 (70.5%), biphasic in 5 (11.4%), desmoplastic in 3 (6.8%), and other variants in 5 (11.4 %). Results: On the result of IHC stains for EGFR, 7 cases (24.1%) showed positive expression. According to the EGFR FISH analysis only 2 cases (11.8%) revealed a positive gene copy number gain of EGFR (high polysomy), both cases were in IHC-positive group. Thirty-five cases of MM did not show any EGFR mutation. EGFR mutation was found in only one case of MM on exon 21, L861. Conclusion: EGFR overexpression is relatively common in epithelioid type of MM. The protein expression of EGFR is not significantly related to a gene copy number gain and nor related to EGFR mutation. However, the further studies to the larger group in future are expected.
Akinwale Damilola Ayodeji
Ladoke Akintola University of technology, Nigeria
Title: Association between secretor status and hepatitis B infection

Biography:
Akinwale Damilola has completed his BSc. in medical laboratory sciences at the age of 27 years from Ladoke Akintola University. He is an intern medical laboratory scientist at Adeoyo maternity teaching hospital, yemetu, Ibadan, Oyo State, Nigeria.
Abstract:
Hepatitis B is an infectious disease caused by the hepatitis B virus (HBV) which affects the liver. It can cause both acute and chronic infections. The aim of this study is to investigate the association between secretor status and Hepatitis B infection. Secretor status was determined by agglutination inhibition method. This study was carried out among 200 subjects, of whom 100 were hepatitis B patients and 100 apparently health subject that served as control. Of the 100 hepatitis B patients, 33(33.0%) were males and 67(67.0%) were females. Of the 33 males, 19 were secretors and 14 were non-secretors while 45 and 22 of the females were secretors and non-secretors respectively. There is no significant association between secretor status and sex (2=1.7, df =1, p= 0.192). This study shows that there is no significant association between secretor status and hepatitis B.

